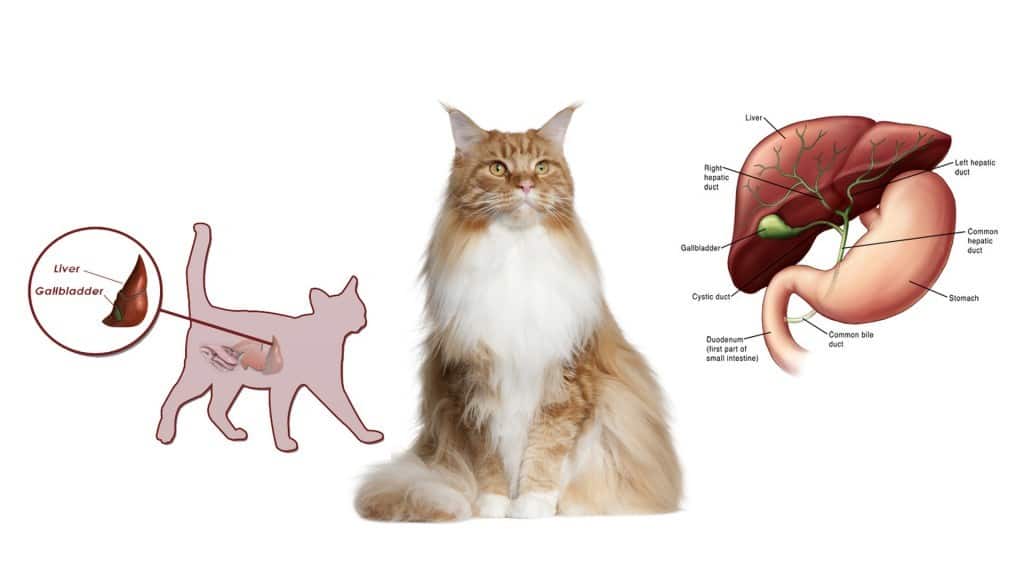
Liver disease in cats is a serious health concern that can have a significant impact on their overall well-being. The liver is a vital organ responsible for metabolizing nutrients, filtering toxins, and aiding in digestion. When the liver becomes diseased, it can disrupt these essential functions, leading to a variety of symptoms and complications. Unfortunately, liver disease is often overlooked until the condition becomes advanced, as the symptoms can be subtle and easily mistaken for other health issues. This blog post will discuss the symptoms, causes, and treatment options for liver diseases in cats, providing essential information for cat owners to better understand and manage this condition.
Symptoms of Liver Disease in Cats
Recognizing liver disease in cats can be difficult due to the nonspecific nature of many symptoms. Some signs may develop gradually, while others may appear suddenly. Common symptoms of liver disease in cats include a noticeable decrease in appetite and weight loss. Loss of appetite is often one of the first indicators that something is wrong, with the cat becoming less interested in food or refusing to eat altogether. This lack of appetite can lead to significant weight loss, especially if the condition goes unnoticed for an extended period.
Jaundice, a yellowing of the skin, eyes, and gums, is another key symptom of liver disease. Jaundice occurs when the liver is unable to process bilirubin, a byproduct of the breakdown of red blood cells. As a result, bilirubin accumulates in the bloodstream, causing the yellow discoloration. Jaundice is often a sign that liver function is severely compromised and should prompt immediate veterinary attention.
Vomiting and diarrhea are also common in cats with liver problems. These gastrointestinal disturbances may occur as a result of liver dysfunction, affecting digestion and the body’s ability to process food properly. Cats may also appear lethargic and weak, lacking the energy to engage in normal activities. This fatigue can interfere with their daily routines, and owners may notice that their cat is sleeping more or seems uninterested in playtime.
In some cases, cats with liver disease may exhibit increased thirst and urination. This can occur because the liver is no longer effectively filtering toxins from the blood, leading to an imbalance of fluids in the body. As a result, the cat may drink more water than usual and need to urinate more frequently. This symptom is often mistaken for other conditions like diabetes or kidney disease, which is why a proper diagnosis is necessary.
Causes of Liver Disease in Cats
Liver disease in cats can be caused by a variety of factors, including infections, toxins, and underlying health conditions. One of the most common causes of liver disease in cats is hepatic lipidosis, also known as fatty liver disease. This condition occurs when fat accumulates in the liver cells, making it difficult for the organ to function properly. Hepatic lipidosis is often triggered by a sudden loss of appetite, typically due to stress, illness, or changes in diet. Overweight cats are particularly at risk, as they are more likely to experience fatty liver disease when they stop eating for even a short period.
Infections can also contribute to liver disease in cats. Bacterial infections, such as leptospirosis, can lead to liver inflammation and damage. Viral infections, such as feline leukemia virus (FeLV) and feline infectious peritonitis (FIP), can also impact the liver. In some cases, fungal infections may be responsible for liver damage as well, although these are less common.
Toxins, both environmental and dietary, are another significant cause of liver disease in cats. Certain medications, such as acetaminophen (Tylenol), are highly toxic to cats and can cause severe liver damage, even in small doses. Other toxins, such as chemicals, plants, and contaminated food, can also lead to liver failure. Cats that ingest or are exposed to toxic substances may experience a rapid decline in liver function, leading to life-threatening consequences if left untreated.
Liver tumors, whether benign or malignant, can also cause liver disease in cats. While tumors affecting the liver are less common than other causes, they can interfere with the liver’s normal functions, leading to symptoms like jaundice, weight loss, and digestive disturbances. Primary liver cancer can develop directly in the liver, while secondary liver cancer occurs when cancer spreads from other organs to the liver.
Chronic inflammation or infection of the bile ducts in the liver, a condition known as cholangitis, can also result in liver disease. This inflammation may be caused by bacterial infections, gallstones, or other underlying issues. Inflammation of the liver can lead to long-term liver damage, making it harder for the organ to perform its essential functions.
Treatment for Liver Disease in Cats
The treatment for liver disease in cats varies depending on the underlying cause and the severity of the condition. A thorough veterinary examination, including blood tests, imaging, and possibly biopsies, is necessary to determine the specific cause of liver disease and develop an appropriate treatment plan.
Dietary changes are often a key component of treatment for liver disease in cats. A special diet designed to support liver health may be recommended, particularly for conditions like hepatic lipidosis. This may include high-protein, easily digestible food, along with supplements to aid digestion and promote healing. In some cases, feeding tubes may be required to ensure the cat receives enough nutrients if they are unwilling or unable to eat on their own.
Medications are also commonly used to treat liver disease in cats. Antibiotics may be prescribed if a bacterial infection is present, while corticosteroids may be used to reduce inflammation in cases of liver damage or autoimmune disease. For cats with fatty liver disease, medications that help break down fat and support liver regeneration may be given. Antioxidants and liver-supporting supplements, such as S-Adenosyl Methionine (SAMe) and vitamin E, are often used to help protect the liver cells from further damage.
Supportive care is critical for cats with liver disease, especially if they are severely ill. This can include fluid therapy to combat dehydration, pain management to make the cat more comfortable, and anti-nausea medications to help manage vomiting and loss of appetite. In severe cases, hospitalization may be necessary to stabilize the cat’s condition and provide intensive care.
In some cases, surgery may be required to treat liver disease. If liver tumors are present, surgical removal may be possible, depending on the size and location of the tumor. However, surgery is typically only an option for tumors that have not spread to other parts of the body. In cases of gallstones or blockages in the bile ducts, surgery may also be needed to restore normal liver function.
Long-term management of liver disease often requires ongoing veterinary care and regular monitoring of liver function. Cats with chronic liver disease may require lifelong dietary modifications and medications to manage their condition. Close communication with your veterinarian is essential to adjust the treatment plan as needed and ensure the best possible outcome for your cat.

Conclusion
Liver disease in cats is a serious condition that requires prompt attention and intervention. Recognizing the symptoms early, such as loss of appetite, jaundice, vomiting, and lethargy, is key to preventing further complications and ensuring that your cat receives the appropriate treatment. The causes of liver disease are varied and can range from infections to toxins, with conditions like hepatic lipidosis and liver tumors being common culprits. Treatment typically involves dietary changes, medications, and supportive care, but the approach will depend on the specific cause of the disease. With early diagnosis and proper care, many cats with liver disease can live long and healthy lives. If you notice any signs of liver issues in your cat, consult with your veterinarian as soon as possible to ensure the best chance for recovery.
